Abstract
Introduction: Paroxysmal nocturnal hemoglobinuria (PNH) is a rare, clonal hematopoietic stem cell disease caused by mutations in an X-linked gene called phosphatidylinositol glycan class A (PIG-A). Venous thromboembolism (VTE) is known to be a leading cause of death in patients with PNH and is considered to be a clinical emergency, warranting treatment with eculizumab and therapeutic anticoagulation. Although several studies have analyzed the overall disease burden and predictors of outcomes associated with VTE in patients with PNH, data on inpatient burden and outcomes are scarce. We sought to investigate the inpatient burden, characteristics and overall outcomes associated with VTE-related complications among patients with PNH using a large nation-wide database.
Methods: The current nation-wide retrospective analysis was conducted using the National Inpatient Sample (NIS), which includes administrative and demographic data from a 20% sample of inpatient hospitalizations in the United States. We interrogated the NIS for admissions among patients with PNH from 2016-2019 using appropriate ICD-10 diagnosis codes. Admissions with known hypercoagulable conditions such as anti-phospholipid antibody syndrome, factor V Leiden mutation, prothrombin gene mutation, protein C and S deficiency, etc. were excluded. Hospitalizations with PNH were further assessed for VTE-related complications using appropriate ICD-10 codes and data on baseline characteristics and inpatient outcomes were collected and analyzed. Chi-square test was used for categorical data and Student's t-test was used for continuous variables. A p-value < 0.05 was considered statistically significant. SAS version 9.4 (SAS Institute Inc.) was used for statistical analysis.
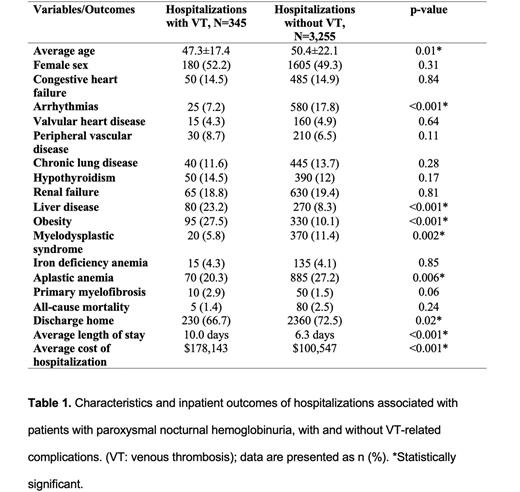
Results: A total of 3,600 hospitalizations were included for analysis, out of which, 345 (9.6%) were associated with VTE. Lower extremity deep vein thrombosis (DVT) was noted to be the most common (100/345, 29%) followed by hepatic vein thrombosis/ Budd Chiari syndrome (80/345, 23.2%), portal vein thrombosis (70/345, 20.3%), pulmonary embolism (60/345, 17.4%), upper extremity DVT (60/345, 17.4%), non-specific VTE (15/345, 4.3%) and renal vein thrombosis (5/345, 1.5%). Table 1 shows baseline characteristics and co-morbidities in hospitalizations associated with and without VTE. Patients in the VTE group were significantly younger (47.3±17.4 vs 50.4±22.1, p=0.01) and had a higher prevalence of co-morbid obesity (27.5% vs 10.1%, <0.001) and chronic liver disease (23.2% vs 8.3%, p<0.001).
The prevalence of myelodysplastic syndrome (5.8% vs 11.4%, p=0.002) and aplastic anemia (20.3% vs 27.2%, p=0.006) was noted to be significantly lower in the VTE group, while no difference was noted with iron deficiency anemia (4.3% vs 4.1%, p=0.85) and primary myelofibrosis (2.9% vs 1.5%, p=0.06). No patients with acute myeloid leukemia could be captured in our cohort in either of the groups. Overall, there was no difference in all-cause inpatient mortality between groups with and without VTE (1.4% vs 2.5%, p=0.24), however, hospitalizations with VTE-related complications were associated with longer average length of stay (10 days vs 6.3 days, p<0.001), higher average cost of hospitalizations ($178,143 vs $100,547, p<0.001) and lower rate of discharge to home (66.7% vs 72.5%, p=0.02).
Conclusions: Overall, 10% of the hospitalizations in our analysis were associated with VTE, out of which, lower extremity DVT, hepatic and portal vein thrombosis were the most common sites (approximately 75% of the VTE burden). Patients with VTE were younger and had a higher prevalence of co-morbid obesity and chronic liver disease. Prevalence of myelodysplastic syndrome and aplastic anemia was noted to be significantly lower in the VTE group, however, further prospective clinical data are needed to analyze the impact of these diagnoses on overall risk of VTE in patients with PNH. Although VTE did not appear to increase all-cause inpatient mortality; associated increase in average length of stay, average cost of hospitalization and decreased likelihood of discharge to home were noted. Concerted efforts to strengthen and enhance care for patients with PNH in the ambulatory setting are needed to prevent inpatient hospitalizations with VTE and reduce associated healthcare burden and costs.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal